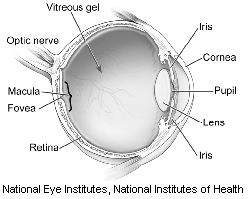
 The macula is the region of the retina anatomically located in the center of the retina. It is responsible for providing the sharp, central vision needed to see fine details. A macular hole is a small full-thickness retinal defect in the macula.
The macula is the region of the retina anatomically located in the center of the retina. It is responsible for providing the sharp, central vision needed to see fine details. A macular hole is a small full-thickness retinal defect in the macula.
Epiretinal membrane (also referred to as macular pucker, surface wrinkling retinopathy, or macular wrinkle) refers to the formation of a semitransparent scar tissue on the surface of the retina. With time, this scar tissue can contract and result in distortion of the underlying retina and/or macular edema (swelling).
Symptoms
People with macular holes may notice:
- Loss of central vision
- Blurred or distorted central vision
This may result in difficulty with reading and driving.
The primary symptom of a macular pucker is distorted vision, but it can also result in decreased vision or loss of central vision.
While most macular puckers do not affect vision and are found during a routine eye examination, about 1 in 3 macular puckers will affect vision and may require surgery.
Causes
Macular holes most often result from aging and “bad luck.” Sometimes the vitreous—the gel that fills the eye—can pull on the retina, resulting in a macular hole. In other instances, a membrane (called an epiretinal membrane) can exert traction on the edges of the center of the macula (the fovea) and result in the formation of a hole.
Unlike age-related macular degeneration (AMD), there is no genetic link to macular hole formation. The same holds true when comparing this condition to diabetic retinopathy, as there is no systemic cause or environmental factor responsible for macular hole formation.
In rare instances, macular holes can occur due to an injury, but most causes of macular holes remain unknown.
If you develop a macular hole in one eye, there is less than a 5% risk of developing a hole in the second eye.
In macular pucker, on the other hand, most cases are idiopathic, meaning there is no identifiable cause. In some instances a macular pucker can develop after a retinal tear or detachment or secondary to a variety of retinal vascular diseases (diabetes or retinal vascular occlusions).
Risk factors
Macular holes are most common in people age 60 or older and seem to be more common in women.
Age is the primary risk factor for the development of macular pucker, but additional risk factors include:
- History of a retinal tear or detachment
- Diabetes
- Retinal venous occlusions
- Inflammation in the eye (uveitis)
Diagnostic tests
The key diagnostic test for identifying macular holes and puckers is optical coherence tomography (OCT). This technology is also very useful in educating the patient on their condition and in assessing response to treatment.
Treatment and drugs
Macular holes can be treated with a surgical procedure called a vitrectomy. During this procedure, the vitreous gel is removed and replaced with a bubble of gas and air. Over the course of a few days to weeks the bubble will help the macular hole close.
Patients may be required to maintain a face-down position for a few days after surgery to help the gas bubble exert pressure on the hole and help it close. The gas bubble will gradually dissolve and leave the eye over a few weeks.
It is important that patients with a gas bubble in their eye not fly or receive inhaled anesthetics during the brief time they have a gas bubble in their eye, as it can result in the pressure in the eye elevating as the bubble expands.
Effectiveness of surgery is on a patient-to-patient basis; however, patients who had macular holes for shorter periods of time tend to heal faster than those who had macular holes for several months or years.
If a macular pucker is severe and results in loss of vision or significant macular wrinkling, the retina specialist may recommend a vitrectomy and membrane peeling, where scar tissue is peeled from the surface of the retina.
Like most surgeries, these procedures carry potential complications:
- Cataract formation
- Re-opening or persistence of the macular hole
- Retinal detachment
- Infection
- Glaucoma
- Bleeding
- In cases of macular pucker, a reformation of the pucker
Smaller macular holes can, in rare instances, heal themselves. If a macular pucker has no significant effect on vision, the retina specialist may not recommend vitrectomy and instead suggest follow-up visits to check vision and repeat OCT scans to look for any progression in the condition.
Prevention
There is no way to prevent a macular hole from forming or a macular pucker from occurring.
